Geographic Information Systems (GIS) have changed how public health works by allowing researchers, policymakers, and healthcare providers to see and understand the links between health issues, the environment, and healthcare resources. This blog post will discuss how GIS can be used to map disease outbreaks and health resources, helping to make informed decisions to improve public health.
The Power of GIS in Public Health
GIS technology enables public health professionals to:
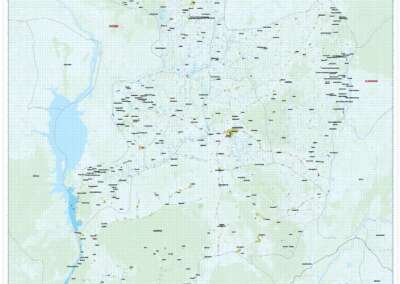
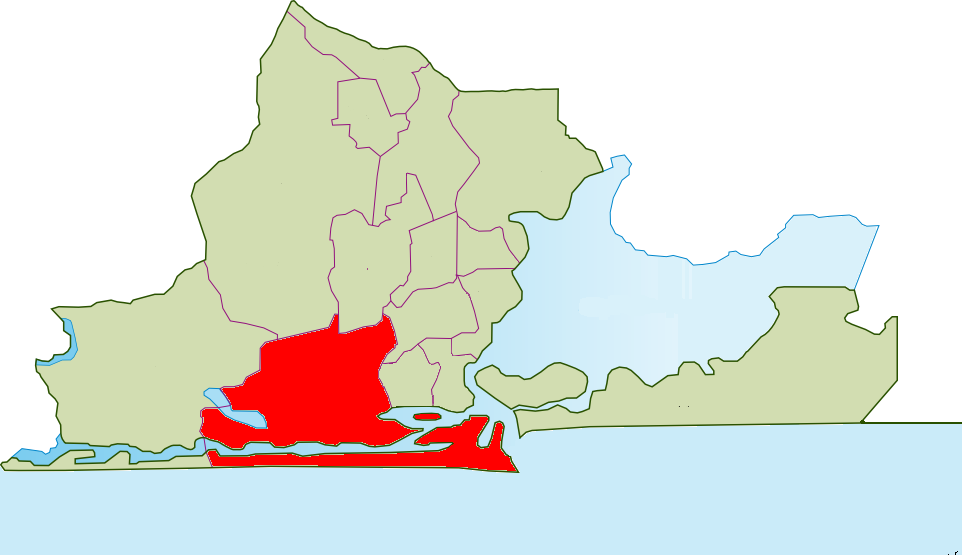
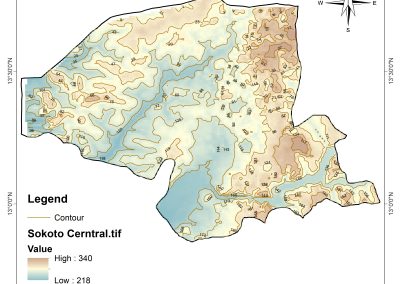
- Visualize Disease Patterns: Create maps that show where diseases are spreading and identify hotspots.
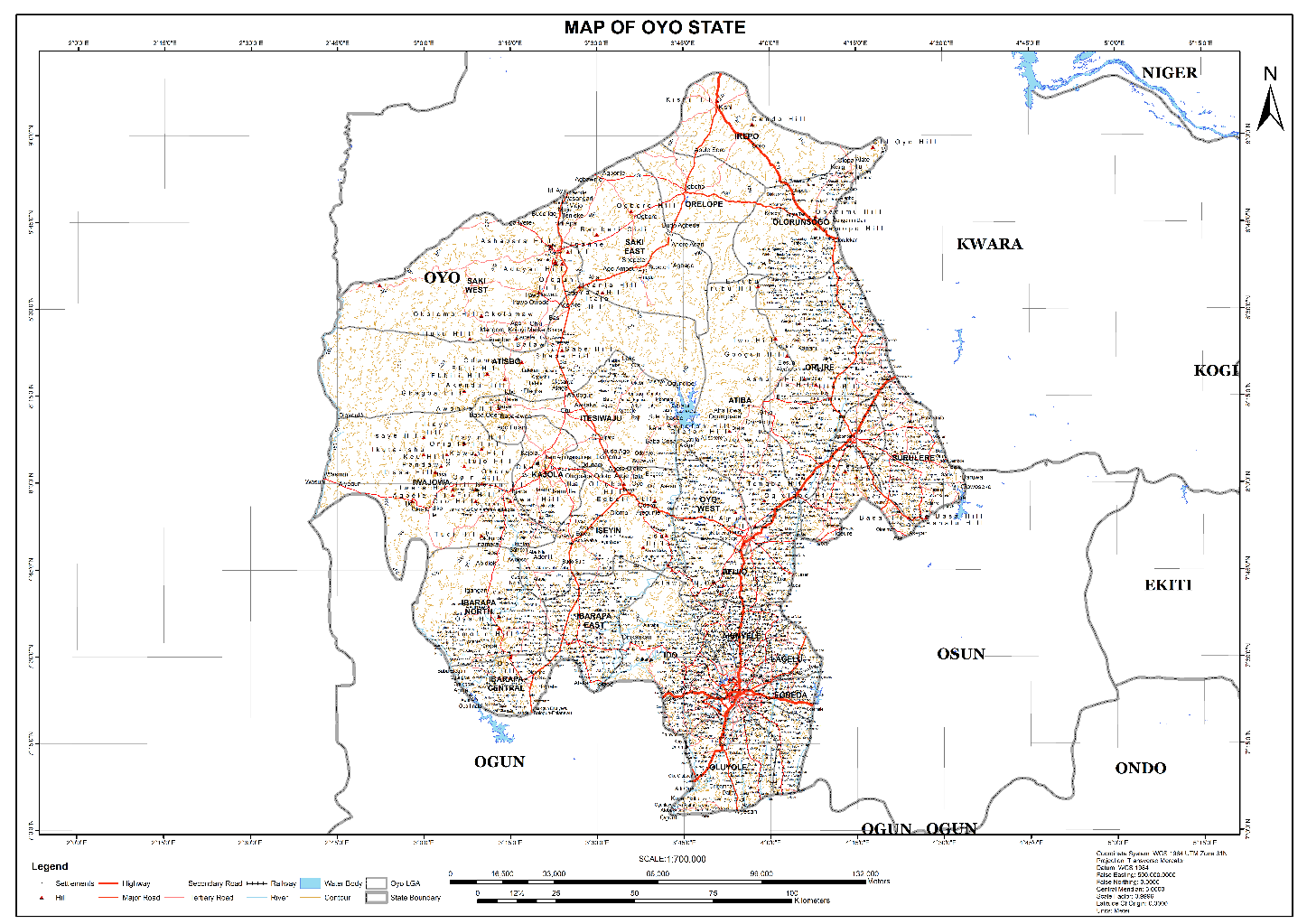
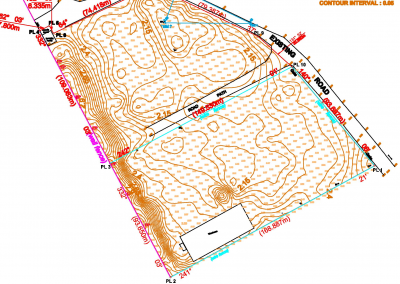
- Analyse Environmental Factors: Study how things like climate and air quality relate to disease outbreaks.
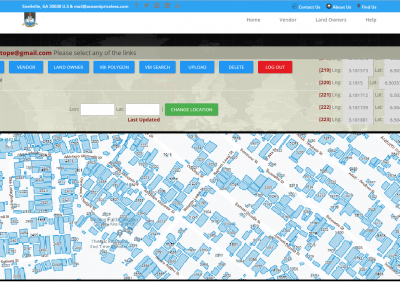
- Optimize Resource Allocation: Find areas with little healthcare access and focus on distributing resources effectively.
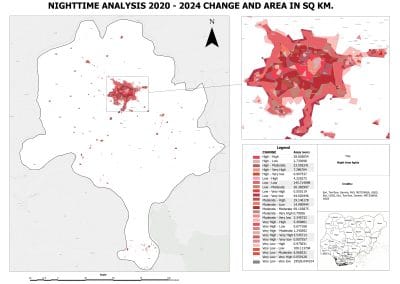
- Track Progress: Monitor changes in disease rates and healthcare outcomes over time.
Mapping Disease Outbreaks
GIS can help to:
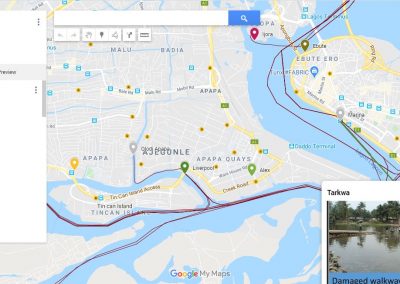
- Identify Clusters: Spot areas where diseases are concentrated.
- Track Transmission: Model how diseases spread and identify potential routes.
- Predict Risk: Identify regions that might be at high risk for disease outbreaks.
Examples of GIS in Disease Outbreak Mapping
– Ebola Outbreak (2014-2016): GIS helped identify hotspots and guided contact tracing.
– Zika Virus Outbreak (2015-2016): GIS showed links between Zika and environmental factors, aiding public health responses.
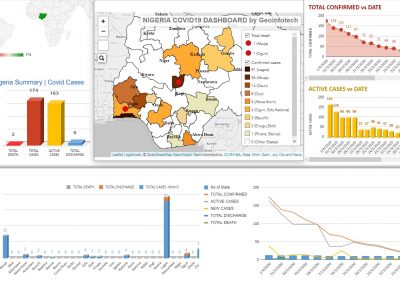
– COVID-19 Pandemic: GIS was essential for tracking cases, hospitalizations, and vaccination efforts.
Mapping Health Resources
GIS also helps to:
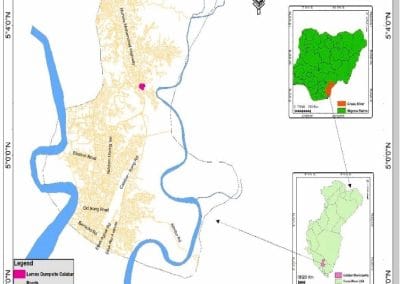
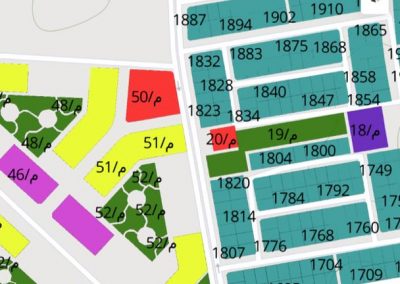
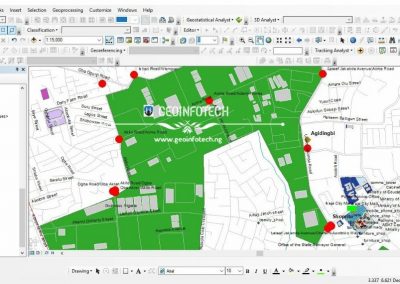
- Identify Healthcare Gaps: Find areas where healthcare services are lacking.
- Optimize Facility Placement: Determine the best locations for new healthcare facilities.
- Allocate Resources: Ensure resources are distributed based on community needs.
Examples of GIS in Health Resource Mapping
– Healthcare Access in Rural Areas: GIS identified regions with limited access, leading to targeted help.
– Hospital Capacity Planning: GIS informed decisions on where to place hospitals and how to expand their capacity.
– Vaccine Distribution: GIS improved the distribution of vaccines during flu seasons.
Best Practices for Implementing GIS in Public Health
To effectively use GIS in public health, consider these best practices:
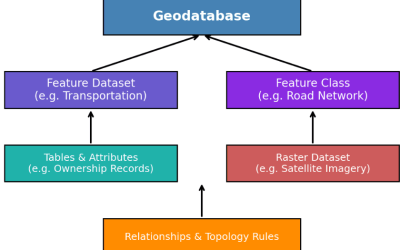
- Integrate Diverse Data Sources: Combine health, environmental, and demographic data for a complete picture.
- Use Spatial Analysis: Apply methods to find patterns in health data.
- Visualize Results: Share findings through clear maps and dashboards.
- Collaborate with Stakeholders: Work with policymakers, healthcare providers, and community leaders to ensure support.
Conclusion
GIS technology has greatly improved public health by providing insights into disease outbreaks and health resource distribution. By using GIS, public health professionals can make better decisions, allocate resources wisely, and ultimately enhance health outcomes. As technology advances, GIS will become even more important for tackling current and future health challenges.